Spider veins and varicose veins are a common disease
You will find detailed information in our vein dictionary

Vein dictionary
The vein dictionary gives you a survey of the most important medical terms concerning vein disease and the treatment of spider veins and varicose veins.
Ambulatory
Treatment or procedure in a doctor’s practice, clinic, or hospital as an outpatient or day patient, not requiring admission to hospital overnight.
Anaesthesia
Temporary loss of sensation, especially of pain and touch; induced by the administration of a drug (an anaesthetic agent).
Anamnesis
Also known as medical history or even as just history, anamnesis is the patient’s clinical history, including past medical events and in particular the history and the course of the present condition.
For example, in the case of varicose veins, the doctor will ask what symptoms you have, how long you have had them, and whether other members of your family have had varicose veins.
Anticoagulants
Medicinal products to inhibit (stop) blood clotting.
Anticoagulation
Inhibition of coagulation (clotting) by taking medicinal products to thin the blood (anticoagulants).
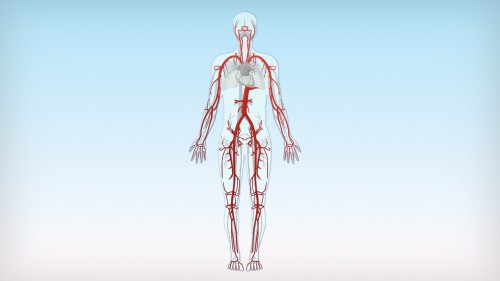
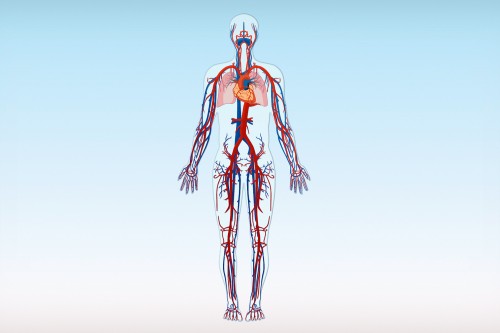
Arteries
Blood vessels that distribute blood from the heart to the body. The heartbeat causes a pulse, which can be felt in the main arteries. Arteries transport bright red blood, rich in oxygen and nutrients, to the tissues and organs.
The pulmonary arteries are the only exception, as they take oxygen-depleted blood from the heart to the lungs.
The largest artery in the human body is the aorta.
Bleeding varicose veins
Acute complication of varicose veins. The vein walls of varicose veins are particularly thin and they often lie very close to the surface. Therefore, the risk of bleeding is very high. Even minor injuries can lead to severe bleeding, because the pressure in the varicose veins is elevated. First aid is to elevate the affected leg, apply a sterile dressing and get the person to the nearest doctor for treatment.
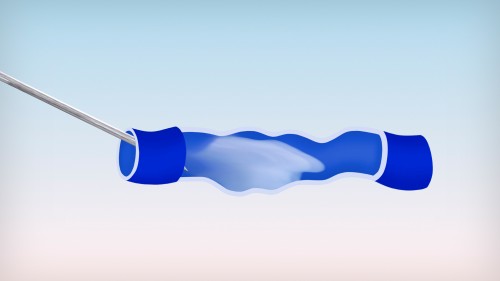
Catheter
Flexible or rigid tubes of different lengths and thicknesses. Usually made of rubber or synthetic material and inserted temporarily into the body to diagnose or treat disease. In the case of varicose veins, for example, a catheter may be inserted into the diseased vein, in order to treat it with laser beams or a sclerosant.
CEAP classification
Is an internationally recognised classification of venous disorders, often used by doctors to describe the disease. Clinical findings are divided into 7 groups (C0 to C6): C0 means no visible signs of venous disease, C1 small varicose veins such as spider veins, C2 varicose veins, C3 varicose veins with oedema, C4 varicose veins with skin changes, C5 healed venous leg ulcers and C6 active venous leg ulcers. In addition, it gives information on the cause of the disease, the vein system affected and the nature of the pathological changes.
CHIVA
Is a special surgical procedure for varicose veins based on the idea that as many veins as possible should be kept for the transport of blood from the leg. The operation is usually performed under local anaesthesia, as several incisions are required. The incisions are not usually so big that the patient needs a general anaesthesia. The procedure is fairly time consuming and disputed among the experts.
Chronic
Permanent or persistent disease. Chronic forms of disease usually develop gradually over a long period of time.
Chronic venous insufficiency
See CVI
Compression therapy
Method of treatment that increases the flow rate of blood and lymph in the direction of the heart by maintaining a constant local pressure on the vessels in the leg. This pressure can be applied with a compression bandage or by wearing compression stockings. Bandages usually have a greater effect.
Compression therapy is used for various conditions, e.g. to relieve the symptoms of varicose veins. The external pressure presses the dilated veins together, allowing the valves to close better, thus improving blood flow to the heart. As varicose veins do not disappear on their own, compression therapy has to be used for the rest of the patient’s life.
As a rule, compression therapy is also applied for a few days or weeks after the treatment of varicose veins, in order to get the best possible results.
Compression therapy is also used to prevent deep vein thrombosis and to treat lymphoedema. In addition, compression bandages can be used as support and fixation bandages after injury or damage to the musculoskeletal system. Rhena-Varidress® and Autosana bandages are particularly suited to this purpose.
Crossectomy
Also called high saphenofemoral or saphenopopliteal ligation. Surgical procedure for varicose veins usually performed under general anaesthesia. The trunk veins are exposed through an incision in the skin, tied off, and cut off at the site where they meet the deep vein system thus interrupting the blood flow. All side branch veins in the area, including the healthy ones, are also cut off during the procedure. Operations on the great saphenous vein (see trunk veins) are performed in the groin and those on the small saphenous vein (see trunk veins) in the hollow of the knee. Surgery at the level of the knee is more complicated than in the groin.
Crossectomy is usually combined with further surgical procedures such as stripping. You may need to stay up to 3 days in hospital after the operation and will generally be off work for 1-2 weeks.
If varicose veins reappear in the same place and further surgery is necessary, the second operation is technically more difficult and associated with significantly more complications.
CVI
Acronym for chronic venous insufficiency. CVI is often the result of untreated varicose veins or deep vein thrombosis and is the most common cause of problems in the legs. CVI is caused by longstanding stasis (pooling) of blood in the legs due to leaky valves in the veins. It causes various complications, some of which may be serious.
Fluid collects in the tissues (oedema), especially around the ankles and lower leg. The legs swell up and the skin often itches or tingles. Eczema and chronic inflammation of the skin can be seen in the later stages. There may also be severe disorders in the supply of nutrients to the tissues. These changes can be seen as leathery-looking hardened or discoloured skin, especially around the ankles and on the lower legs. Without proper treatment, poorly-healing open wounds known as venous leg ulcers or stasis ulcers may develop in these areas.
Deep vein thrombosis of the leg
Thrombus formation (blood clot) in the deep veins of the leg. The veins may be completely or partially occluded (blocked) by the clot. When the clot only partially occludes the vein, the body’s natural factors can usually dissolve it with time.
Deep vein thrombosis (DVT) of the leg can give rise to pain and swelling of the calf or leg, but may not cause any symptoms at all. Thrombosis may occur in various medical conditions, such as heart disease and cardiac failure, after operations, or spontaneously. In addition, DVTs may occur if someone is bedridden or not moving the legs during a long-distance flight (economy class syndrome). There is a particular risk of developing thrombosis if the blood flow in the vein is slow and the vein wall is damaged. Platelets accumulate at the damaged site and clump together to form a blood clot. Therefore, thrombosis may develop in untreated varicose veins and with thrombophlebitis.
In the worst case scenario, thrombosis gives rise to pulmonary embolism, when a piece of the clot breaks off and is washed away by the blood until it reaches the lungs, where it blocks blood vessels. Pulmonary embolism may be fatal if the essential vessels in the lungs are occluded.
The diagnosis of DVT can be made with an ultrasound scan. Treatment usually consists of anticoagulants (medicinal products to thin the blood) and compression therapy; sometimes medicinal products are given to dissolve the clot or surgery is performed. DVTs are usually associated with destruction of the valves in the vein, with the result that blood flow in the direction of the heart is no longer guaranteed. CVI (chronic venous insufficiency) may develop as a result.
Deep veins
The veins of the deep vein system. As the name implies, they lie deep within the tissues between the muscles in the legs, and transport most of the venous blood back to the heart. Valves in the deep veins may be incompetent (leaky) after deep vein thrombosis, for example, or with longstanding severe varicose veins that have not been treated. The result is chronic venous insufficiency (CVI).
Diagnosis
Determining which disease is present by assigning the specific findings to the respective condition. The aim of the diagnostic investigation of varicose veins is to identify their nature and extent, in order to decide on the best treatment strategy. The diagnosis of varicose veins is made with the aid of the patient’s anamnesis (medical history), a physical examination, and Doppler or duplex ultrasound.
Doppler ultrasound
Also called Doppler ultrasonography or Doppler sonography. It is a painless and bloodless procedure for diagnosis. It measures the rate of blood flow in the vessels.
First of all, gel is spread over the relevant area of skin. This is necessary as any air trapped between the ultrasound probe and the skin would interfere with the examination.
The ultrasound probe sends out ultrasound waves which pass through the skin to reach the blood vessels. If these sound waves hit blood cells in the vessels, some of the waves are reflected back with a different frequency. This change in frequency depends on the movement of the blood cells and thus allows the flow direction and the velocity of the blood cells to be measured. The results can be displayed in various ways, for example, as an audible signal or as the flow rate on a monitor.
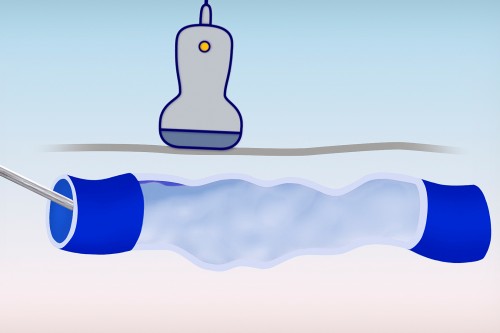
Duplex ultrasound
Also known as duplex ultrasonography or duplex sonography, this is a painless and bloodless procedure for diagnosis. It provides more information about the vessels than Doppler ultrasound. Colour duplex ultrasound scanning is the most modern method of examination and is ideally implemented not only for diagnostic investigations, but also to monitor progress and treatment after sclerotherapy or operations.
As with Doppler ultrasound, gel is spread over the relevant area of skin before the examination. This is necessary as any air trapped between the ultrasound probe and the skin would interfere with the examination of the blood vessels.
Duplex ultrasound is a combination of routine ultrasound imaging of the tissues (black/white imaging) and Doppler ultrasound (measurement of blood flow). It can be used to look at both superficial and deep veins, arteries, and the surrounding tissue on the screen. It is also possible to display the rate and direction of the blood flow within the vessels in different colours. This provides important information on thrombosis, disorders of the valves, the extent of disease, and the prognosis of the vein problems.
Duplex ultrasound guided sclerotherapy
State-of the-art sclerotherapy procedure for treating large varicose veins. Guided by duplex ultrasound, the sclerosant is injected into the diseased segments of the veins under visual control. It is often used in combination with foam sclerotherapy. The sclerosant foam is clearly visible in the ultrasound image, so that its distribution in the vein can easily be followed.
Eczema
A skin disease, usually itchy, that manifests itself as an inflammatory skin reaction. There are often red patches, vesicles (tiny blisters), nodules, or scaly skin. It is not infectious. Along with hardening of the skin, discolouration, and poorly healing ulcers, eczema is often found in the ankle and lower leg area in advanced stages of untreated varicose veins and in association with chronic venous insufficiency (CVI).
Embolism
Partial or complete closure of a blood vessel by a plug (abnormal particle) transported in the blood stream. The plug may consist of a thrombus (blood clot). A piece of the clot breaking off and being carried to the lungs is one of the most dangerous complications of a deep vein thrombosis; this condition is called pulmonary embolism. If the blood clot suddenly blocks off a main pulmonary artery, the circulation in the lungs collapses and, in the worst case, the outcome may be fatal.
Treatment consists of medicinal products to thin the blood (anticoagulants).
The prevention of pulmonary embolism by preventing thrombosis is a medical priority. Prevention consists of exercise, anticoagulants, compression therapy, and the elimination of varicose veins.
Endovenous therapy
Procedures used successfully in contemporary non-surgical treatment of varicose veins, including large varicose veins. Using radiofrequency or laser energy, diseased veins are burned and closed off by heat. These methods are therefore referred to as thermal procedures. They do not require a general anaesthesia, but are usually carried out with tumescent anaesthesia (a special type of local anaesthesia). Another endovenous procedure is sclerotherapy, when a liquid or foamed sclerosant is injected into the diseased vein and the vein is permanently closed. Sclerotherapy can be carried out without any anaesthesia at all.
Exercise
Exercise is always good for the veins and is the simplest way of preventing varicose veins. People with healthy veins and those with venous insufficiency need exercise, as this activates the muscle pump, which helps to transport blood from the legs back to the heart. Walking, hiking, cycling, Nordic walking, swimming, and all types of sporting activities that require the legs to work without over-exerting them can help to prevent venous problems and reduce symptoms.
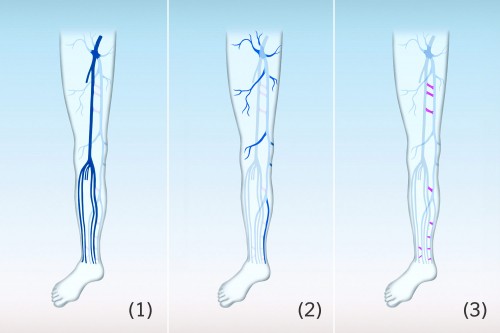
Foam sclerotherapy
This state-of-the-art endovenous therapy has revolutionised the treatment of varicose veins. While sclerotherapy with liquid sclerosant is the treatment of choice for spider veins and reticular varicose veins, foam sclerotherapy is particularly suitable for larger varicose veins of the side branch and trunk veins. According to the guidelines of the German Society of Phlebology, foam sclerotherapy is a good alternative to surgery, laser therapy, and radiofrequency ablation therapy.
Foam sclerotherapy employs foam instead of a liquid sclerosant to inject into the vein. Immediately before treatment, the doctor produces foam from the tried-and-tested liquid sclerosant containing polidocanol (lauromacrogol 400) as active substance. Sclerotherapy with sclerosant foam is carried out under ultrasound guidance, so that the doctor can clearly see the varicose veins and the distribution of the foam in the vein. The sclerosant foam is injected directly into the varicose veins, where it sticks the vein walls together strongly (obliteration and sclerosis). Unlike treatment with liquid sclerosant, the foam is not diluted with blood or carried away as quickly in larger veins. This is especially important in large varicose veins, as it allows the foam to act longer on the vein wall.
The body gradually breaks down the obliterated veins over the following weeks, ideally without leaving any remnants. These treated veins are not needed for transporting the blood back to the heart. After treatment, the blood returns to the heart without any problem via the deep vein system.
The use of foam generally requires lower concentrations and smaller quantities of sclerosant and treatment goals are usually achieved more quickly.
In addition, foam sclerotherapy is almost painless, minimally invasive, and can be performed rapidly on an outpatient (ambulatory) basis. After foam sclerotherapy, patients can resume their normal daily activities immediately and return to work without delay.
General anaesthesia
For a general anaesthesia, the administration of a medicinal product induces an artificial sleep-like state resulting in a temporary loss of consciousness and loss of sensation of pain. Anaesthesia may also be given as a regional anaesthesia, where the patient remains awake, but there is no sensation of pain in a particular part of the body. Surgical procedures invariably require some form of anaesthesia. Sclerotherapy, on the other hand, does not need any anaesthesia at all.
Glue
Product to treat trunk varicose veins that is still in the research phase. Unlike the well-established methods of treatment that have proved themselves with time, there are hardly any clinical studies on glue as yet and certainly no long-term results.
Using a special device, a cyanoacrylate adhesive (like instant glue) is injected at multiple sites into the affected trunk veins under local anaesthesia, in order to stick the vein walls together. The glue remains in the body and should be broken down with time. Treatment costs about 2400 EUR per leg.
The glue is not offered as a medicinal product, but rather as a medical device. Bringing a medical device onto the market requires less extensive investigation and fewer clinical studies than are needed to obtain marketing authorisation for a medicine. Health authorities are very strict about safety monitoring for medicinal products and it is stringently regulated to ensure maximum safety for patients.
No final conclusions can be drawn on the long-term efficacy and safety of glue used for this purpose, as few patients with varicose veins have as yet been treated with this method.
Great saphenous vein (vena saphena magna)
See trunk veins
Haematoma
Accumulation of blood in the tissues caused by bleeding from the blood vessels, for example after injury, injection, or surgery.
Haemorrhoids
Haemorrhoids are often wrongly considered to be varicose veins of the bottom. Everyone, however, has this ring-like vascular cushion in the anus (back passage) that helps to keep the end of the bowel properly closed. Having haemorrhoids is therefore a normal and not a diseased state. It only becomes a disease (called haemorrhoidal disease) when the vascular cushion is enlarged and causes symptoms. When someone says “I’ve got haemorrhoids” they actually mean the disease, commonly known as piles. Once the vascular cushion is enlarged, it rarely shrinks on its own. Haemorrhoidal disease may cause bleeding during bowel movements as well as itching, burning, and a foreign body sensation. Left untreated, the condition progresses and gives rise to a mucus discharge. Sclerotherapy is one way of treating haemorrhoidal disease.
Heparins
A class of medicinal products used to inhibit blood coagulation (clotting) in the short term. They are anticoagulants. Heparins are given to prevent deep vein thrombosis in bed-ridden patients and prior to operations.
History
See anamnesis
Hyperpigmentation
Localised increased brown colour of the skin. The brownish discolouration may develop in the region of untreated varicose veins. It may also temporarily occur after treatment of varicose veins as the so-called “ghost of the veins”. That is to say, the veins have been successfully obliterated (closed off) and are now being broken down in the body. During this time, a slight brown discolouration appears where the diseased vein used to be.
Imaging
Imaging is very important for the diagnosis of venous diseases, as it allows us to take a look inside the veins.
Modern non-invasive ultrasound displays and identifies pathological (abnormal) changes in the veins and their valves. The use of colour allows us to see where the blood flows and how quickly. Before the introduction of these modern techniques, phlebography was the best way of investigating the leg veins. This technique involves an X-ray examination, in which contrast medium is injected into a vein. Through the contrast medium, the veins and any pathological changes can then be seen. Today phlebography is only used in special cases that cannot be diagnosed by any other means.
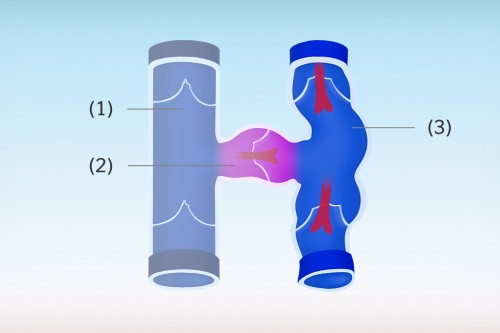
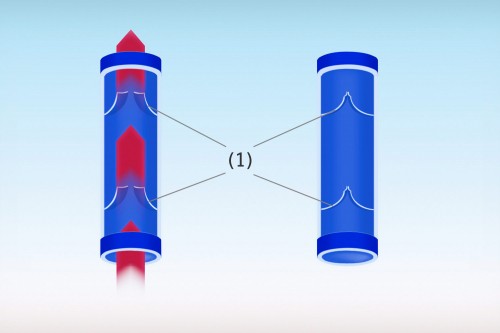
Incompetent valves
Impaired function or loss of function of the valves in the superficial or deep veins. The valves no longer close properly and are not able to control the direction of flow. Incompetent (leaky) valves allow the blood to flow in the wrong direction under the force of gravity. Blood pools in the veins. The pressure in the vessels increases continuously until they dilate and ultimately develop varicose veins.
Insufficiency
Impaired function, weak function, or loss of function. Venous insufficiency occurs when the valves in the veins are incompetent (leaky) – that is to say, they no longer close tightly and not all the venous blood is directed solely towards the heart. Blood refluxes through the incompetent valves and pools in the legs, causing the affected veins to dilate (balloon out). Varicose veins develop.
Intermittent compression
Also called intermittent pneumatic compression. Treatment to relieve stasis (pooling) that is used when there is oedema. The affected limb, for example the leg, is enclosed by a sleeve with inflatable air chambers and pressure is applied by alternately inflating and deflating the chambers. This promotes the flow of blood and lymph in the right direction towards the heart and helps to reduce fluid accumulation (oedema) in the tissues. To be successful, this therapy must be applied regularly and often in combination with compression stockings.
Irreversible
Not possible to reverse, cannot be changed back.
Laser
The word is derived from the first letters of the phrase “light amplification by stimulated emission of radiation”. The name “laser” thus describes a relatively complicated procedure in physics and is used for the device with which the beams are produced as well as for its physical effect.
Laser beams are electromagnetic waves that hit human tissues as strongly bundled beams. Depending on the duration and intensity of the exposure, the thermal effects range from slight warmth to carbonisation of the tissue.
Lasers have a wide range of uses today, but must always be used properly. For example, shining a laser pointer into someone’s eyes may damage their eyesight.
Lasers are basically medical devices and not medicinal products (medicines).
Besides surgical methods, radiofrequency ablation therapy, and foam sclerotherapy, laser therapy has proved useful in the treatment of trunk varicose veins. It is also referred to as endoluminal or endovenous laser therapy (EVLT). Treatment usually costs in the region of 1500 EUR.
A special catheter is first inserted into the diseased vein under ultrasound guidance and the laser fibre is then pushed through the catheter. A laser beam is emitted through the fibre and the vein closed step by step by gently and continuously pulling back the fibre. The diseased vein is in effect burnt. The area treated has to be kept cool because of the heat generated during the procedure. Burns, scabbing, and scars may occur if the area is not adequately cooled or the laser system is not adjusted correctly.
Laser therapy can be performed as an outpatient (ambulatory) procedure and does not need a general anaesthesia. Instead, tumescent anaesthesia (a special form of local anaesthesia) is used. Tumescent anaesthesia builds a fluid firewall around the veins that prevents heat from being transmitted to the surrounding tissues and causing damage to nerves and vessels.
It is more difficult to push the catheter through tortuous snake-like varicose veins, as found in side branch veins, without perforating the vein. Other methods are usually to be preferred in such cases.
Small lasers may sometimes be used to treat spider veins in the legs. It is not, however, the method of choice and is very painful. Sclerotherapy is the method of choice for spider veins.
Lipodermatosclerosis
A chronic inflammatory reaction of the skin and subcutaneous tissues, usually seen on the lower leg. It may develop with chronic venous insufficiency (CVI) and is characterised by painful indurated (hardened) skin around the leg and red or brown skin discolouration. The skin is easily injured and wound healing is delayed. There is a greatly increased risk of venous leg ulcers.
Local anaesthesia
A form of anaesthesia. The targeted use of a local anaesthetic in a particular area makes it temporarily insensitive to pain and touch. In contrast to general anaesthesia, the patient stays awake. A local anaesthesia may need one or more injections.
Local anaesthetics
Medicinal products that are used for local anaesthesia.
Lymph
Slightly cloudy body fluid. Lymph flows in its own system of vessels called lymphatics, lymphatic vessels, or lymph channels. Together with the veins, these channels drain waste products from the tissues. Swelling of the legs is not always due to venous problems, but may also be caused by blockage of the lymph drainage.
Lymphoedema
Swelling due to stasis (pooling) of lymph in the lymph channels. Excess lymph enters the tissues and accumulates there. Lymphoedema is usually seen in the legs or arms.
Medical device
Objects or substances that are used to cure or prevent disease. Medical devices may be objects that do not come into direct contact with the body or skin, such as syringes, but also substances and devices that are introduced into the body, such as catheters that are inserted into the veins for endovenous therapy. From the safety point of view, it is important to distinguish between medical devices and medicinal products (medicines), as the requirements for marketing authorisation (permission to bring on to the market) and safety monitoring are very differently regulated. The requirements for medical devices are generally less stringent. It is therefore often disputed in court whether a product is truly a medical device or whether it is not, in fact, a hidden medicinal product.
Medicinal products have pharmacological effects, that is to say, their effects are due to interactions with the cells in the body. Basically, medical devices may have only a purely physical effect and not react with the body. This distinction is not easy to understand and often not completely clear. In any case, a medicinal product is more intensively scrutinised by the authorities.
Medical history
See anamnesis
Medicinal product
Also called medicines, medications, pharmaceuticals, and drugs. Substances or preparations of substances that are, as a rule, intended to cure, relieve, or prevent disease. Medicines have pharmacological effects, that is to say, their effects are due to interactions with the body’s cells. Medicinal products can only be sold when they have been approved by the health authorities. This marketing authorisation is based on numerous studies of the medicine’s efficacy and safety. Pharmaceutical manufacturing is regulated by many national and international laws and medicinal products are closely examined before they may be sold. In addition, medicinal products are continuously monitored and reviewed to ensure maximum safety for the patient.
Micro-sclerotherapy
 Sclerotherapy of small varicose veins is also called micro-sclerotherapy. It is an outpatient (ambulatory) method used to treat spider veins and reticular varicose veins without lasers, anaesthesia, or surgery. A specially developed medicinal product, the sclerosant, is injected directly into the diseased vein through a very fine needle. Inside the varicose vein, the sclerosant reacts with the vein wall. Normal processes in the body cause the walls to stick together, thus closing the vein so that blood no longer pools in the dilated vein. The body gradually converts the diseased vein into connective tissue and it disappears with time.
Sclerotherapy of small varicose veins is also called micro-sclerotherapy. It is an outpatient (ambulatory) method used to treat spider veins and reticular varicose veins without lasers, anaesthesia, or surgery. A specially developed medicinal product, the sclerosant, is injected directly into the diseased vein through a very fine needle. Inside the varicose vein, the sclerosant reacts with the vein wall. Normal processes in the body cause the walls to stick together, thus closing the vein so that blood no longer pools in the dilated vein. The body gradually converts the diseased vein into connective tissue and it disappears with time.
 More than one treatment session may be needed, depending on the size and number of the varicose veins to be treated. Patients can resume their normal activities immediately after sclerotherapy and return to work without delay. Compression stockings should be worn for a few days after micro-sclerotherapy.
More than one treatment session may be needed, depending on the size and number of the varicose veins to be treated. Patients can resume their normal activities immediately after sclerotherapy and return to work without delay. Compression stockings should be worn for a few days after micro-sclerotherapy.
According to the German Society of Phlebology guidelines, sclerotherapy is the method of first choice for treating spider veins and small varicose veins.
Mini-sclerotherapy
See micro-sclerotherapy
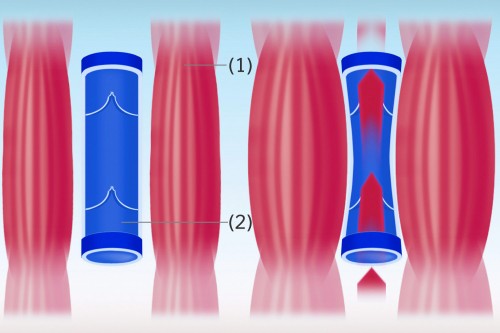
Muscle pump
Besides the valves, the so-called muscle pump has a major role in transporting blood from the legs to the heart. The deep veins in the leg are surrounded by muscles; muscular activity, such as walking or even just moving the foot, tenses and thickens the muscles.
In this way, the surrounding muscles put pressure on the veins and force the blood out of them. With functional valves, blood can flow in one direction only, that is to say, towards the heart, as the valves prevent it from flowing back towards the feet. A distinction is made between the different muscle pumps of the soles of the feet, the ankles, the calves, and the thighs depending on the muscle group involved.
Non-invasive
An investigation or a treatment procedure that can be performed without puncturing the skin or cutting into the body.
Certain procedures that involve the smallest possible damage on entry to the body (for example, needle punctures) are termed minimally invasive.
Oedema
Watery fluid leaves the blood vessels or lymphatics and accumulates in the tissues. Oedema causes painless swelling of the affected tissues and is often called “water in the legs”. Various diseases may cause ankle and leg oedema, e.g. heart or kidney disease. The legs may also swell up in the advanced stages of varicose veins or other venous system disorders. Oedema due to venous disease is characterised by indentation with pressure; that means it retains a visible impression of a finger after it had been pressed firmly into the tissues. Oedema tends to be worse in warm weather and towards the end of the day. Swelling is also noticeable after wearing socks with narrow elastic cuffs all day – a deep circular groove around the leg can be seen when the socks are taken off.
Oedema-protective agents
Medicinal products (medicines) that are used in venous disease to prevent or reduce oedema. With venous disease such as varicose veins there are changes in the vein walls, which make them more permeable to components of the blood. As a result, fluid collects in the tissues around varicose veins – the so-called oedema.
Oedema-protective agents reduce the pathological (abnormal) permeability of the vein wall and counteract oedema. This relieves the symptoms of venous weakness, such as swelling of the ankles or legs and a feeling of tension, pain, or heaviness in the legs. These agents are most effective when the medicine is already taken before oedema develops.
The active substances include horse chestnut seed extract and troxerutin (e.g. Troxeven® in Germany). The effects of troxerutin in reducing permeability help to prevent fluid accumulation in the tissues and stabilise the blood vessels, especially the veins. In general, the use of an oedema-protective agent supports, but cannot and should not replace professional medical treatment from a doctor
Operation
Invasive surgical procedure on the body with the help of medical instruments. The aim of an operation is to restore diseased tissue or to remove diseased and damaged tissue. The procedure starts with an incision and is generally performed under a general anaesthesia.
Surgery for varicose veins includes crossectomy (high saphenofemoral ligation), stripping, and phlebectomy.
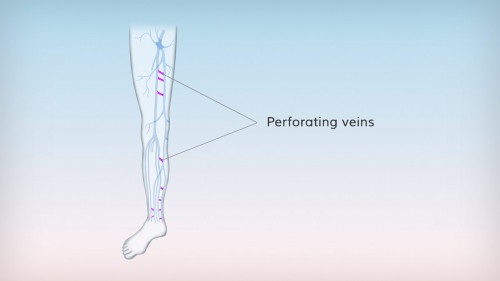
Perforating veins
Also called perforators. The veins in the leg are divided into superficial and deep veins. The two systems are linked at various sites by connecting veins known as perforating veins. Perforating veins have valves and are responsible for venous blood flowing from the superficial into the deep veins.
Perforating veins can also become varicose veins. Non-functioning valves allow the reverse flow of blood from the deep veins through the perforating veins, leading to stasis (pooling of blood) in the superficial veins.
Phlebectomy
Surgical procedure to remove side branch varicose veins and less commonly also reticular varicose veins. Also called hook phlebectomy.
The procedure is usually performed under local anaesthesia, whereby the local anaesthetic is injected along the varicose veins. A hook is inserted through a small skin incision into the subcutaneous tissue, where the diseased veins run. The vein is caught with the hook, pulled out through the skin, and ripped off under the skin. Another incision is made, the hook inserted again, the next segment of the vein ripped out, and so on. In this way, it is possible to remove large segments of vein through several small incisions. The incisions usually heal without scarring.
Phlebectomy is often performed as an outpatient (ambulatory) procedure and leads to only minor restrictions at work and in everyday life following the operation.
Haematomas and bruises of varying severity occur in the area of the operation, but these usually disappear within a few days.
Phlebography
Before the introduction of modern ultrasound scanning, phlebography was the best means of visualising the leg veins and important for diagnosis of varicose veins. This X-ray examination involves injecting contrast medium (dye) into a vein to make the vein and any pathological changes visible. Today, phlebography is only performed in special cases that cannot be diagnosed by other means.
Phlebologist
Vein doctor, vein specialist. A phlebologist is a doctor who specialises in diseases of the veins.
In Germany, phlebologists have usually qualified initially in the specialties of surgery, dermatology, general practice medicine, or internal medicine.
The necessary knowledge in phlebology is gained during 1½ years of specialist training under an authorised superior with a great deal of experience in the field.
Phlebology
Medical subspecialty concerned with the prevention, diagnosis, and treatment of venous diseases of the legs.
Doctors with a qualification in phlebology are required to have undergone standardised specialist training.
Photoplethysmography
Also called by its acronym PPG or light reflexion rheography (LRR). Painless and bloodless procedure for diagnosis of venous disease with infrared light. It determines the refill time of the veins, which allows their condition and function to be assessed. A sensor is placed on the inside of the lower leg. The patient sits down and is asked to raise and lower the toes 10 times to activate the muscle pump and transport the blood in the leg veins towards the heart. This action empties the veins. The foot is then held still and the veins refill relatively slowly if they are healthy. With venous disease, the valves do not close properly and the blood flows backwards, filling the veins much more quickly than is the case if the veins are healthy. The shorter the refill time, the more severe the venous disease. The refill time in healthy legs is more than 25 seconds, but refilling takes less than 10 seconds with severe venous disorders.
Post-thrombotic syndrome
Post-thrombotic syndrome is a complication with persistent damage in the deep vein system of the legs after deep vein thrombosis has resolved. The thrombosis has damaged or even destroyed the valves in the affected area. The deep veins are no longer able to function properly and chronic stasis (pooling of blood) occurs in the leg. This initially causes a feeling of heaviness or aching in the legs, with swelling and pain. Varicose veins, skin discolouration, chronic inflammation of the skin, and venous leg ulcers may develop with time.
Prophylaxis
The prevention of disease. In the case of varicose veins, prophylaxis is also considered to be a delaying of their development. It is always worthwhile, because in most cases there is an inherited predisposition and our modern lifestyle contributes to the development of varicose veins. Weight control and exercise is the key. Sporting activities such as gymnastics, swimming, Nordic walking, and cycling activate the muscle pump. Wearing compression stockings and taking oedema-protective agents are also advisable. After showering in the morning, the legs should always be given a short cold shower starting at the feet and working up to the thighs; this closes the vessels again and the legs feel lighter. However, the success of prophylactic measures depends on their regular use. In any case, go and see your general practitioner or a vein specialist (phlebologist) at the first sign of varicose veins and especially if you have any acute symptoms in the legs.
Pulmonary embolism
See embolism
Radiofrequency ablation therapy
Along with laser therapy and foam sclerotherapy, radiofrequency ablation therapy is one of the endovenous therapy procedures that have become well-established in the treatment of trunk varicose veins. The method is also referred to as endoluminal or endovenous radiofrequency ablation and radiofrequency-induced thermal therapy (RFITT).
Treatment costs up to 1500 EUR. The method is similar to laser therapy, except that the damage to the veins is caused by radio waves. A catheter is inserted into the diseased vein under ultrasound guidance. Radio waves are emitted via the catheter tip and the vein closed off step by step while continuously pulling back the catheter. Radiofrequency ablation is gentler than laser therapy, but even here, temperatures in the diseased vein reach up to 100° and it is in effect burnt. Similarly to laser therapy, burns, scabbing, and scars may also occur with radiofrequency ablation if the tissues are not adequately protected from the heat. Tumescent anaesthesia (a special type of local anaesthesia) is used to prevent overheating. This anaesthesia method builds a fluid firewall around the veins that prevents heat from being transmitted to the surrounding tissues and causing damage. A general anaesthesia is usually not necessary and the treatment is often performed as an outpatient (ambulatory) procedure.
It is more difficult to push the catheter through tortuous snake-like varicose veins, such as those found in side branch veins, without damaging them. Other methods are usually preferable in such cases.
The catheter and equipment used in this method of treatment are medical devices and not medicinal products.
Recurrence
Relapse, reappearance of a disease. In the case of varicose veins, there is no treatment for the underlying connective tissue weakness, so the reappearance of such veins, for example, after surgery, is due to the development of new varicose veins. Furthermore, if treatment is incomplete, veins that were initially closed open up again, disconnected veins sometimes grow again, or a collateral (by-pass) circulation develops. In principle, varicose veins are a progressive disease and cannot be completely cured by any known treatment. So there is always the possibility of new varicose veins developing.
Reflux
Backwards flow. Reflux in varicose veins means the abnormal flow of blood through incompetent valves back into the segments of the vein nearer the feet (in the wrong direction).
Reticular varicose veins
Small varicose veins in the skin, with a diameter of 1-3 mm; they are slightly larger than spider veins and often occur together with them.
They tend to form fan-like or net-like patterns and are often found on the sides of the upper and lower leg. They are usually bluish in colour and can be seen clearly. Many people find them cosmetically unattractive.
Very pronounced reticular varicose veins, in particular, may cause physical symptoms and they may be the first signs of venous insufficiency that will become steadily worse with time. Go and see your general practitioner or a vein specialist (phlebologist) if you find that you have any reticular varicose veins.
Sclerotherapy is one method that can be used to treat reticular veins safely and effectively.
Saphenofemoral junction (SFJ), saphenopopliteal junction (SPJ)
The SFJ is an arching region in the groin where the great saphenous vein (see trunk veins) meets the deep vein system. The old term “crosse”, which is rarely used in English today, comes from the French expression for a bishop’s crook.
Several superficial veins also join the deep vein system in the region, giving the junction a star-like appearance.
The region where the small saphenous vein (see trunk veins) meets the popliteal vein at the knee is known as the saphenopopliteal junction (SPJ).
Saphenous veins
See trunk veins
Sclerosant
Also called a sclerosing agent. A sclerosant is a medicinal product used for sclerotherapy of varicose veins of all sizes – trunk, side branch, and perforating varicose veins as well as reticular varicose veins and spider veins.
Sclerosants effectively obliterate the varicose veins. The best-known sclerosant contains the active substance polidocanol (lauromacrogol 400). The doctor injects it directly into diseased veins, using it as either a liquid or foam. Inside the varicose vein, the sclerosant reacts with the vein wall. The body’s natural processes cause the vein walls to stick together and close off the vein, so that blood can no longer pool in the diseased vein. The body gradually converts the obliterated vein into connective tissue and it disappears with time.
Sclerosants are medicinal products that the health authorities will only authorise to be sold if comprehensive studies on their good efficacy and safety are available.
Sclerosant foam
Used in foam sclerotherapy to treat varicose veins. Instead of the liquid sclerosant employed in conventional sclerotherapy, a special foam is injected into the diseased veins. Immediately before treatment, the doctor produces the foam from the liquid sclerosant by using a specially developed syringe system.
Foam sclerotherapy is performed under ultrasound guidance, allowing the foam to be injected under visual control and the subsequent distribution of the foam to be followed exactly. The foam has a powerful adhering effect causing the vein walls to stick together (obliteration and sclerosis). The body gradually breaks down the obliterated veins over the following weeks, ideally without leaving any remnants behind.
Unlike treatment with liquid sclerosant, the foam is not diluted with blood and carried away so quickly in larger veins. This is particularly important in large varicose veins, as it allows the foam to act longer on the vein wall. Thus, large varicose veins can be treated even more effectively with smaller quantities of sclerosant. Sclerotherapy of large varicose veins with foam usually achieves the treatment goals quicker: the obliteration and elimination of the diseased veins.
Sclerosing agent
See sclerosant
Sclerotherapy
Also called obliteration, sclerotherapy is a minimally invasive procedure for treating varicose veins, in which a sclerosant is injected to obliterate and eliminate pathological (diseased) veins. Sclerotherapy is a method that has long proved its worth in the ambulatory treatment of varicose veins of all sizes – trunk, side branch, and perforating varicose veins as well as reticular varicose veins and spider veins.
The principle is simple: using a fine needle, the sclerosant – as either a liquid or foam – is injected directly into the diseased vein. Inside the varicose vein, the sclerosant reacts with the vein wall. The body’s natural processes cause the vein walls to stick together and close off the vein, so that blood can no longer pool in the diseased vessel. The body slowly converts the obliterated vein into connective tissue and it disappears with time. The functional result of sclerotherapy is equivalent to that of surgery for varicose veins.
These treated veins are not needed for transporting the blood back to the heart. After treatment, the blood returns to the heart without any problem via the deep vein system.
Depending on the number and size of veins to be treated, more than one treatment session may be needed for optimal success. Sclerotherapy is the treatment of choice for spider veins and reticular veins and is also called micro-sclerotherapy. With larger varicose veins, foam is often used instead of a liquid sclerosant, as sclerosant foam has an even more powerful effect. Foam sclerotherapy of trunk varicose veins is a good and cost-effective alternative to surgical procedures and to laser or radiofrequency ablation therapy.
The unattractive varicose veins can be removed by sclerotherapy on an outpatient basis without the use of lasers, surgery, or a general anaesthesia. Treatment is effective, safe, and usually painless.
After sclerotherapy, patients can resume their normal daily activities immediately and return to work without delay.
In addition, sclerotherapy is an effective treatment for haemorrhoids and varicose veins of the oesophagus.
SFJ/SPJ incompetence
Pathological reflux (backwards flow) of blood from the deep vein system across the saphenofemoral junction (SFJ) or saphenopopliteal junction (SPJ) into the trunk veins through valves that are incompetent (leaky). Valves in healthy veins allow the blood to flow in one direction only, that is to say, towards the heart. When they are leaky, the blood also flows in the opposite direction, towards the feet. Blood collects in the legs and varicose veins develop.
Side branch varicose veins
Side branch or tributary varicose veins develop when the valves in the side branch veins are incompetent (leaky) and when the blood flows backwards and dilates the veins. They often occur together with or arise from trunk varicose veins, but may also develop in isolation. Side branch varicose veins tend to have a very tortuous, snake-like appearance and are often clearly visible as bulges under the skin.
Side branch veins
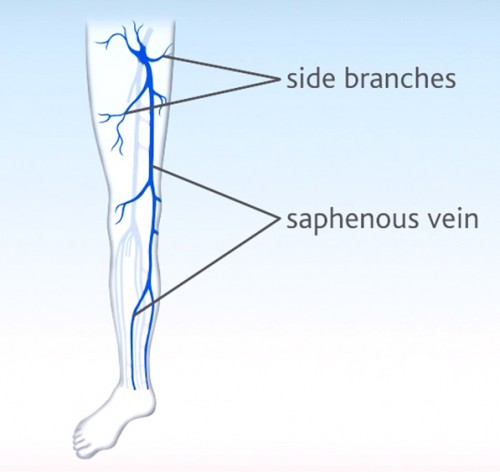 Also called side branches or tributary veins, side branch veins are large superficial veins that empty into the trunk veins.
Also called side branches or tributary veins, side branch veins are large superficial veins that empty into the trunk veins.
The side branch veins run through the lower leg and the thigh; there are many veins connecting them with each other and also to the deep vein system. Side branch varicose veins may develop if their valves are incompetent (leaky). The term “side branch veins” is not really accurate: strictly speaking, trunk veins do not give off branches, but rather the blood comes from the side branch veins emptying into the trunk veins. For the sake of simplicity, however, “side branch veins” continues to be used, as it is such a well-established term.
Small saphenous vein (vena saphena parva)
See trunk veins
Spider veins
Very small varicose veins lying in the skin, with a diameter of less than 1 mm. The bluish or reddish-purple dilated veins can be seen shining clearly through the skin, particularly on the lower leg and the sides of the thighs. More than 60% of adults in Germany have spider veins. They may appear dotted, stripy, fan shaped, or star-like. So they are also called thread veins, star bursts, and telangiectasia. Spider veins may occur singly or in clusters and cover a relatively large area on the leg. They are not always merely an aesthetic or cosmetic problem. Particularly the pronounced spider veins may cause symptoms and be the first visible sign of venous insufficiency that will become worse with time. They may occur in isolation or together with larger varicose veins. If you have spider veins, it is better to err on the side of caution and get your general practitioner or a vein specialist (phlebologist) to have a look at them.
Stripping
Classic surgical procedure to remove varicose veins affecting the trunk veins. In some countries, this treatment is still the gold standard for trunk varicose veins, but in many others it has been superseded by endovenous therapy.
According to the guidelines of the German Society of Phlebology, foam sclerotherapy is a good alternative to surgery, laser, and radiofrequency ablation therapy.
Stripping is usually combined with cutting off other veins in the groin (known technically as crossectomy or high saphenofemoral ligation).
You may need to stay up to 3 days in hospital after the operation and be off work for 1-2 weeks.
The operation for trunk varicose veins is usually performed under a general anaesthesia. The surgeon makes an incision (several centimetres long) in the groin, identifies the point where the trunk vein empties into the deep vein system, then ties off and cuts off the vein. A metal wire is pushed down through the trunk vein to the end of the diseased area, and then brought out through the skin via another incision in the thigh or lower leg. The lower end of the diseased vein is fixed to the wire and then the wire is pulled out, bringing the varicose vein with it. During this procedure, any smaller veins emptying into the trunk vein are ripped off. The wound is closed with sutures.
If varicose disease recurs in the same place and further surgery is necessary, the second operation is technically more difficult and associated with more complications.
Surgery
Medical specialty dealing with the treatment of disease and injuries by surgery (operations) on the living body. Often involves the partial or complete removal of diseased organs or vessels.
Thrombectomy
Surgical removal of a thrombus (blood clot) from a blood vessel.
Thrombophlebitis
Thrombophlebitis is the technical term for inflammation of the superficial veins and often occurs when there are varicose veins. The inflammation causes local warmth, pain, redness, and swelling at the affected site. In some circumstances, the vein can be felt as an indurated (hard), painful thread or nodule.
Consult your doctor if you have any signs of thrombophlebitis, as it may lead to a deep vein thrombosis.
Thrombus
A thrombus is a blood clot in a vessel.
Tributary veins
See side branch veins
Troxerutin
See oedema-protective agents
Trunk varicose veins
Also called truncal varicose veins. These are varicose veins of the trunk veins (great saphenous vein and/or small saphenous vein) in the leg. Varicose veins develop when there are incompetent (leaky) valves in the trunk veins, allowing some of the blood to flow in the opposite direction (to the feet) and pool in the leg veins. Different stages of disease can be identified on the basis of the extent of the reflux, which the doctor can establish when the patient is standing up (backwards flow to only just below the SFJ, to just above the knee, to below the knee, or down to the ankle).
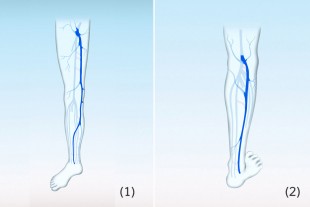
Trunk veins
Also known as saphenous veins or truncal veins. Each leg has two trunk veins, the great and the small saphenous veins. These important vessels of the superficial vein system lie slightly deeper in the connective tissue beneath the skin.
The great saphenous vein (Latin: vena saphena magna), formerly called the long saphenous vein, is the longest vein in the leg and runs up the inside of the leg from the medial malleolus of the ankle across the knee to the groin, where it empties into the deep vein system.
The small saphenous vein (Latin: vena saphena parva), formerly known as the short saphenous vein, runs from the outside of the ankle to just above the hollow of the knee, where it empties into veins of the deep vein system.
Incompetent valves in these superficial veins will cause trunk varicose veins.
Tumescent anaesthesia
A special type of local anaesthesia, in which a large volume of fluid is injected under pressure into the subcutaneous fat tissues. The fluid contains a local anaesthetic agent.
In the case of certain heart diseases, the condition may worsen as a result of the considerable fluid volume burden.
Tumescent anaesthesia is also used in operations on varicose veins and in particular in laser and radiofrequency ablation therapy. It provides a wide area of anaesthesia around the veins to be treated and affords protection from pain. In addition, the large volume of fluid in the tissues acts as a sort of firewall between the vein being treated and the surrounding tissues, especially nerves. This protection has proved particularly effective against burns and thermal damage during laser therapy and radiofrequency ablation.
Ulcus cruris
See venous leg ulcers
Ultrasound
Ultrasonography or sonography. Bloodless procedure used in medicine for the purpose of diagnosis, employing ultrasound waves from outside the body to visualise the structures within. Doctors can use ultrasound to assess blood flow in the vessels. See also: Doppler and duplex ultrasound.
Valve
Connective tissue structure in the veins. When the leg veins transport oxygen-depleted blood back to the heart, they have to work against gravity. The veins contain valves to make sure that the blood flows in the right direction. The valves open when blood flows through towards the heart, but close when it starts to flow in the wrong way.
Therefore, the valves make sure that the blood can flow in only one direction – and that is towards the heart. With varicose veins or chronic venous insufficiency (CVI), the valves no longer function properly and are unable to close tightly (incompetent valves). Blood sometimes flows in the wrong direction back down the legs and pools in the veins there. Left untreated, it causes irreversible damage to the veins with subsequent complications.
Varicose disease
The technical term used for the condition of suffering from varicose veins is varicose disease or varicosis. The condition is chronic and progressive, that is to say, there is no permanent cure. Even after varicose veins have been successfully treated, new ones may develop and require further treatment.
This does not mean that there is nothing you can or should do about it. The treatment options available today can bring varicose disease under control and prevent the complications of longstanding untreated varicose veins, which may sometimes be serious.
Varicose veins (in the legs)
Varicose veins, also sometimes called varicosities, are pathologically enlarged superficial veins, often appearing as snake-like or nodular structures in the legs. They lie in or closely beneath the skin and are therefore usually clearly visible. Varicose veins often bulge out of the skin.
Small varicose veins include spider veins and reticular varicose veins; larger varicose veins involve the side branch veins (side branch varicose veins) or trunk veins (trunk varicose veins).
Varicose veins develop when the veins dilate because of a congenital weakness in the connective tissue and the valves can no longer close tightly and can thus no longer fulfil their valve function. Gravity forces the blood to flow in the wrong direction and it pools in the legs (stasis).
As a result, the pressure in the veins increases continuously until varicose veins develop.
About 60% of adults in Germany suffer from spider veins and reticular varicose veins, while 30% have larger varicose veins. Left untreated, the disease progresses, with discolouration and chronic inflammation of the skin. In the worst cases, thrombophlebitis, deep vein thrombosis, and venous leg ulcers occur. Varicose veins are therefore a common disease that should be taken seriously.
Varicosis
See varicose disease
Varicosities
See varicose veins (in the legs)
Vascular surgery
Subspecialty of surgery, concerned with diseases of the blood vessels, such as varicose veins.
Vein doctor
See phlebologist
Vein specialist
See phlebologist
Vein system
The leg veins can be divided into superficial and deep veins or into the superficial and deep vein system. The superficial veins run in and just beneath the skin. They transport blood from the skin and subcutaneous tissues into the deep vein system, accounting for some 10% of the blood carried back to the heart from the legs. The deep vein system lies deeper inside the leg and is responsible for about 90% of the return blood flow. The superficial and deep systems are joined together at certain points by perforating veins.
Veinlite
Small portable vein finder. It functions by means of the transillumination technique and detects superficial veins that are hardly visible to the naked eye. The device is placed on the skin and reveals even the smallest veins that are difficult to inject. In particular, this means that spider veins and their feeder veins can be targeted more precisely for sclerotherapy, giving even better treatment results.
Veins
Veins are the blood vessels that transport blood from the body back to the heart. Venous blood is dark red, containing less oxygen and more waste products than arterial blood. The pulmonary veins are the only exception, as they carry oxygen-rich blood from the lungs back to the heart.
Veins contain valves to ensure that the blood from the legs returns to the heart against the force of gravity.
Vena saphena magna
See trunk veins
Vena saphena parva
See trunk veins
Venous leg ulcers
Open, usually weeping wounds on the lower leg or foot, which frequently do not heal for a long time. These wounds are called venous leg ulcers, venous ulcers or stasis ulcers. The technical term is ulcus cruris. In most cases, longstanding untreated varicose veins and/or chronic venous insufficiency (CVI) are responsible for venous leg ulcers. The basic cause of this serious complication is a poor healing tendency with a deficient circulation and a poor supply of nutrients to the affected tissues. The acute trigger is often a minor injury to the previously damaged skin. Venous leg ulcers are usually colonised with bacteria and often show signs of inflammation in the surrounding skin.
Venous occlusion plethysmography
Venous occlusion plethysmography (VOP) is a painless and bloodless examination to investigate vein function.
A strain gauge attached to the limb measures changes in volume when the venous outflow is suddenly occluded. The leg veins are first of all filled to the maximum by inflating a blood pressure cuff to prevent venous return. If the veins are healthy, they can additionally take up a certain volume of blood. It is referred to as the venous capacity and is normally 2.5-5ml/100ml tissue. When varicose veins are present, they are dilated and can hold more blood than normal.
The blood pressure cuff is then deflated and the venous blood flows out of the legs. Normal venous blood drainage is 35-100 ml/100ml tissue. Rapid drainage shows that the veins are patent (open). If a vein is occluded (blocked), by thrombus for example, the blood takes longer than normal to drain away.
Vessels
The vessels provide the channels for carrying blood or lymph around the body. Lymph vessels transport lymph and blood vessels transport blood.
Blood vessels are divided into arteries, capillaries, and veins.
Vessels carrying blood from the heart into the body are called arteries. The arteries contain bright red blood that is rich in oxygen and nutrients. The pulmonary arteries are the only exception, as they carry oxygen-depleted blood from the heart to the lungs.
Arteries branch continuously to end in very fine capillaries, where oxygen, nutrients, and waste products are exchanged between the blood and the tissues. Oxygen and nutrients are released from the capillaries into the tissues and waste products from the tissues are taken up into the capillaries.
The blood then reaches the veins. The veins collect the blood, which is now dark red, oxygen-depleted, and contains large quantities of waste products, and transport it back to the heart. The pulmonary veins are the only exception, as they carry oxygen-rich blood from the lungs to the heart. The leg veins have the difficult task to return the blood to the heart against the force of gravity.